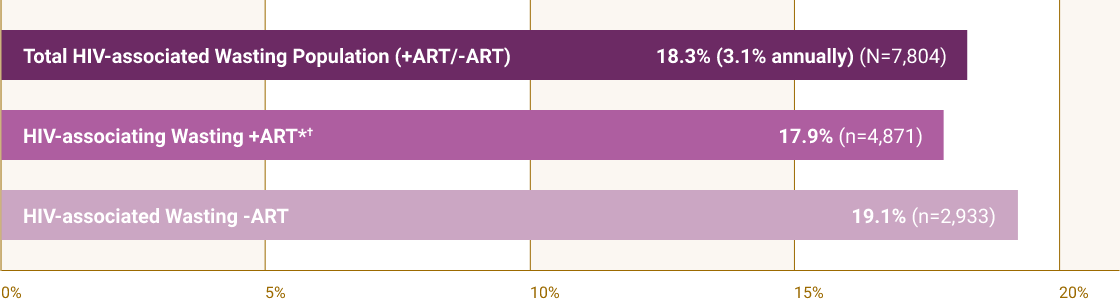
Recent data suggest HIV-associated wasting (HIVAW) is still prevalent in the US and is associated with an increased risk of mortality1,2
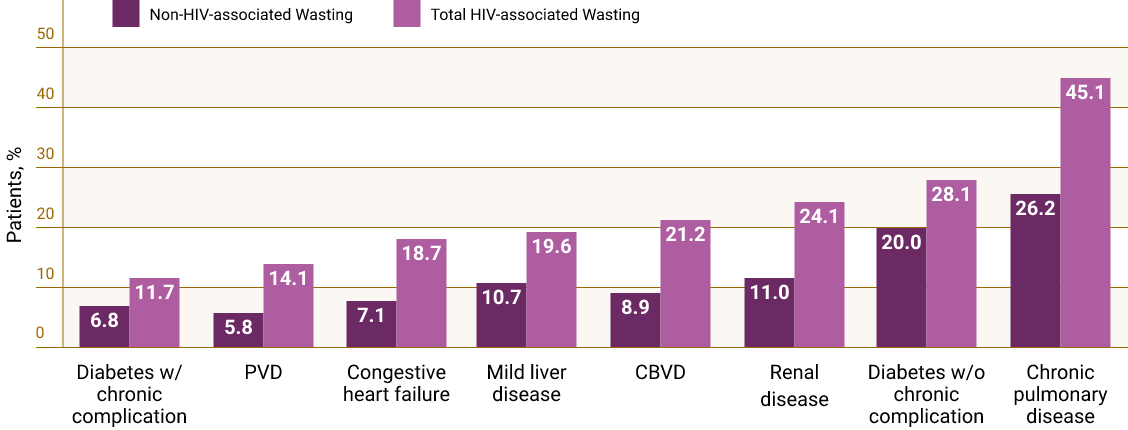
As HIV treatment advances and the management of persistent chronic comorbidities is prioritized, HIVAW, as a disease state, should not be overlooked.